28 Jan How sleep affects our overall wellness part 2
How sleep affects our overall wellness part 2
Welcome to our Post, on week 13 we are sharing part two of the importance of sleep. Here we have focused on research from authorities in this matter and we wish for you to find the answers that you are seeking either to share with a friend a family member or use for yourself, so many people are affected by restless sleep I know personally many of them and it amazes me that even very young people are having sleepless nights.
I-RAMA does not intend to prescribe or replace the advice of your health practitioner before you make any changes please consult with him or her, we are sharing studies and extensive research with the intention to provide you with insights from professionals that are qualified to do so.
We thank you for your loyalty and all the support and kind comments that we receive daily, without it we won’t be here from all of us at I-RAMA.
Reset Your Circadian Rhythms – And Sleep Well
What is Healthy Sleep?
from: https://sleepfoundation.org/sleep-news/what-healthy-sleep
You know that sleep is vital to your physical and mental health. But, how can you tell whether you’re truly sleeping well? Especially if you work shifts, your sleep probably does not look exactly like other peoples’ sleep. It can be hard to measure your sleep patterns against those of the people around you.
On average, adults should optimally receive between seven and nine hours of sleep each night, but those needs vary individually. For example, some people feel best with eight consecutive hours of sleep, while others do well with six to seven hours at night and daytime napping. Some people feel okay when their sleep schedule changes, while others feel very affected by a new schedule or even one night of insufficient sleep.
Here are some statements about your sleep. If these apply to you, it’s a good sign that your sleep is on track. If you’re a shift worker and you don’t agree with many of these, it could mean that you need to make changes in your behaviors and routines to improve your sleep.
You fall asleep within 15-20 minutes of lying down to sleep.
You regularly sleep a total of seven to nine hours in a 24-hour period.
While in your bed, your sleep is continuous—you don’t have long periods of lying awake when you wish to be sleeping.
You wake up feeling refreshed as if you’ve “filled the tank.”
You feel alerted and are able to be fully productive throughout the waking hours (note, it’s natural for people to feel a dip in alertness during waking hours, but with healthy sleep, alertness returns).
Your partner or family members do not notice any disturbing or out of the ordinary behavior from you while you sleep, such as snoring, pauses in breathing, restlessness, or otherwise nighttime behaviors.
Shift workers who try to sleep during the day often wake up after fewer than seven to nine hours, because of the alerting signals coming from their circadian system. This does not mean they don’t need seven to eight hours of sleep per day—it just means it’s harder to sleep during the day. Over time, this can lead to chronic sleep deprivation.
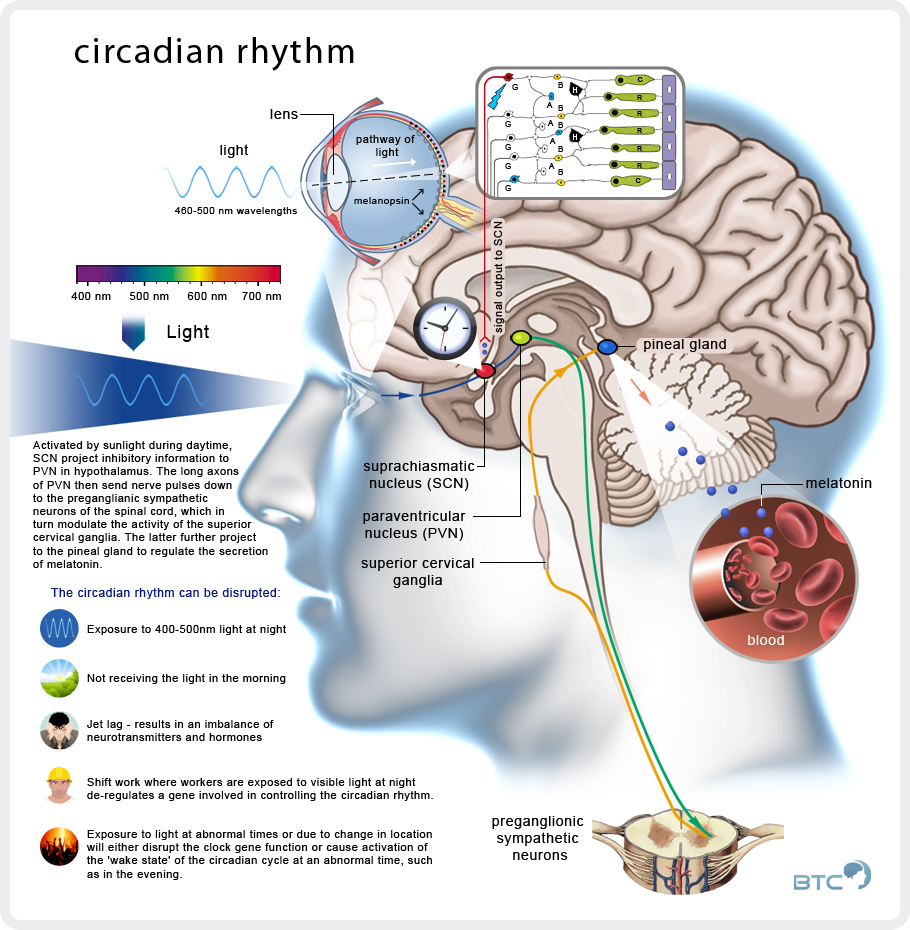
Circadian Rhythm
 Sleep Drive and Your Body Clock
Sleep Drive and Your Body Clock
According to https://sleepfoundation.org/sleep-topics/sleep-drive-and-your-body-clock
Most people notice that they naturally experience different levels of sleepiness and alertness throughout the day, but what causes these patterns? Sleep is regulated by two body systems: sleep/wake homeostasis and the circadian biological clock.
When we have been awake for a long period of time, sleep/wake homeostasis tells us that a need for sleep is accumulating and that it is time to sleep. It also helps us maintain enough sleep throughout the night to make up for the hours of being awake. If this restorative process existed alone, it would mean that we would be most alert as our day was starting out and that the longer we were awake, the more we would feel like sleeping. In this way, sleep/wake homeostasis creates a drive that balances sleep and wakefulness.
The circadian rhythm dips and rises at different times of the day, so adults’ strongest sleep drive generally occurs between 2:00-4:00 am and in the afternoon between 1:00-3:00 pm, although there is some variation depending on whether you are a “morning person” or “evening person.” The sleepiness we experience during these circadian dips will be less intense if we have had sufficient sleep, and more intense when we are sleep deprived. The circadian rhythm also causes us to feel more alert at certain points of the day, even if we have been awake for hours and our sleep/wake restorative process would otherwise make us feel more sleepy.
Changes to this circadian rhythm occur during adolescence when most teens experience a sleep phase delay. This shift in teens’ circadian rhythm causes them to naturally feel alerted later at night, making it difficult for them to fall asleep before 11:00 pm. Since most teens have early school start times along with other commitments, this sleep phase delay can make it difficult to get the sleep teens need — an average of 9 1/4 hours, but at least 8 hours. This sleep deprivation can influence the circadian rhythm; for teens the strongest circadian “dips” tend to occur between 3:00-7:00 am and 2:00-5:00 pm, but the morning dip (3:00-7:00 am) can be even longer if teens haven’t had enough sleep, and can even last until 9:00 or 10:00 am.
The circadian biological clock is controlled by a part of the brain called the Suprachiasmatic Nucleus (SCN), a group of cells in the hypothalamus that respond to light and dark signals. From the optic nerve of the eye, light travels to the SCN, signalling the internal clock that it is time to be awake. The SCN signals to other parts of the brain that control hormones, body temperature and other functions that play a role in making us feel sleepy or awake.
In the mornings, with exposure to light, the SCN sends signals to raise body temperature and produce hormones like cortisol. The SCN also responds to light by delaying the release of other hormones like melatonin, which is associated with sleep onset and is produced when the eyes signal to the SCN that it is dark. Melatonin levels rise in the evening and stay elevated throughout the night, promoting sleep.
In teenagers, research has shown that melatonin levels in the blood naturally rise later at night than in most children and adults. Since teens may have difficulty going to bed early to get enough sleep, it can help to keep the lights dim at night as bedtime approaches. It can also help to get into bright light as soon as possible in the morning.
Circadian disruptions such as jet lag put us in conflict with our natural sleep patterns since the shift in time and light cues on the brain force the body to alter its normal pattern to adjust. This is why jet lag can leave travelers feeling poorly and having more difficulty thinking and performing well. But these symptoms can also occur in everyday life when the circadian rhythm is disrupted by keeping long and irregular hours. Because of this, it is important to keep a regular sleep schedule and allow plenty of time for quality sleep, allowing these two vital biological components — the sleep/wake restorative process and the circadian rhythm — to help us perform at our best.
Natural Sleep Cycles
 According to http://healthysleep.med.harvard.edu/healthy/science/what/sleep-patterns-rem-nrem
According to http://healthysleep.med.harvard.edu/healthy/science/what/sleep-patterns-rem-nrem
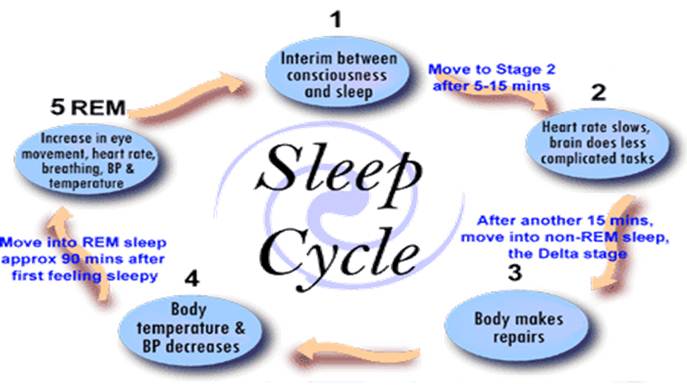
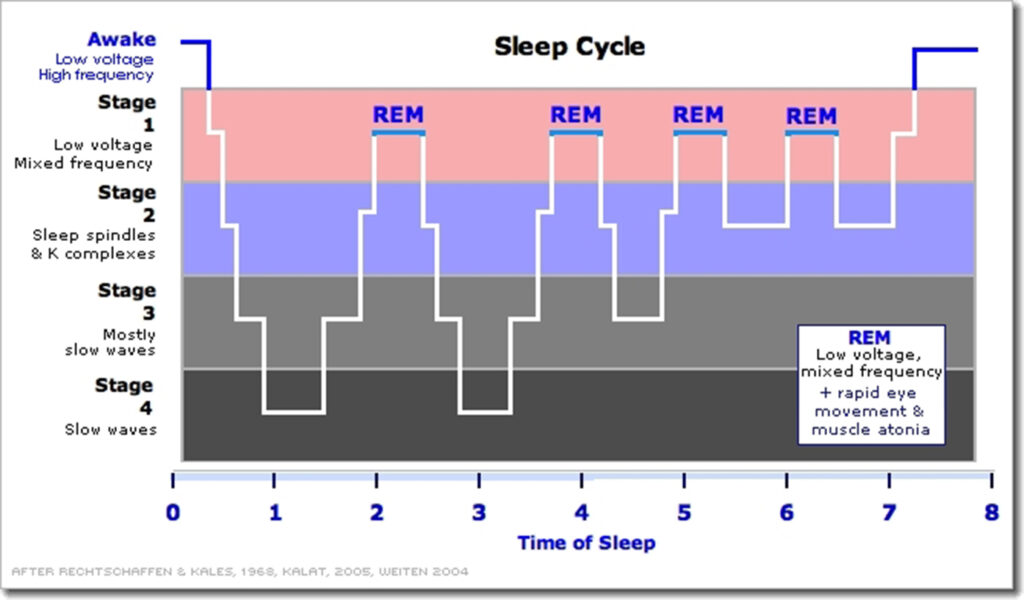
In 1929, an invention that enabled scientists to record brain activity challenged this way of thinking. From recordings known as electroencephalograms (EEGs), researchers could see that sleep was a dynamic behavior, one in which the brain was highly active at times, and not turned off at all. Over time, sleep studies using EEGs and other instruments that measured eye movements and muscle activity would reveal two main types of sleep. These were defined by characteristic electrical patterns in a sleeping person’s brain, as well as the presence or absence of eye movements.
The two main types of sleep are rapid-eye-movement (REM) sleep and non-rapid-eye-movement (NREM) sleep. On an EEG, REM sleep often called “active sleep,” is identifiable by its characteristic low-amplitude (small), high-frequency (fast) waves and alpha rhythm, as well as the eye movements for which it is named. Many sleep experts think that these eye movements are in some way related to dreams. Typically, when people are awakened from REM sleep, they report that they had been dreaming, often extremely vivid and sometimes bizarre dreams. In contrast, people report dreaming far less frequently when awakened from NREM sleep. Interestingly, during REM sleep muscles in the arms and legs are temporarily paralyzed. This is thought to be a neurological barrier that prevents us from “acting out” our dreams.
NREM sleep can be broken down into three distinct stages: N1, N2, and N3. In the progression from stage N1 to N3, brain waves become slower and more synchronized, and the eyes remain still. In stage N3, the deepest stage of NREM, EEGs reveal high-amplitude (large), low-frequency (slow) waves and spindles. This stage is referred to as “deep” or “slow-wave” sleep.
In healthy adults, sleep typically begins with NREM sleep. The pattern of clear rhythmic alpha activity associated with wakefulness gives way to N1, the first stage of sleep, which is defined by a low-voltage, mixed-frequency pattern. The transition from wakefulness to N1 occurs seconds to minutes after the start of the slow eye movements seen when a person first begins to nod off. This first period of N1 typically lasts just one to seven minutes. The second stage, or N2, which is signalled by sleep spindles and/or K-complexes in the EEG recording, comes next and generally lasts 10 to 25 minutes. As N2 sleep progresses, there is a gradual appearance of the high-voltage, slow-wave activity characteristic of N3, the third stage of NREM sleep. This stage, which generally lasts 20 to 40 minutes, is referred to as “slow-wave,” “Delta,” or “deep” sleep. As NREM sleep progresses, the brain becomes less responsive to external stimuli, and it becomes increasingly difficult to awaken an individual from sleep.
Following the N3 stage of sleep, a series of body movements usually signals an “ascent” to lighter NREM sleep stages. Typically, a 5- to 10-minute period of N2 precedes the initial REM sleep episode. REM sleep comprises about 20 to 25 percent of total sleep in typical healthy adults.
NREM sleep and REM sleep continue to alternate through the night in a cyclical fashion. Most slow-wave NREM sleep occurs in the first part of the night; REM sleep episodes, the first of which may last only one to five minutes, generally become longer through the night. During a typical night, N3 sleep occupies less time in the second cycle than the first and may disappear altogether in later cycles. The average length of the first NREM-REM sleep cycle is between 70 and 100 minutes; the average length of the second and later cycles is about 90 to 120 minutes. The reason for such a specific cycling pattern of NREM and REM sleep across the night is unknown. Some scientists speculate that specific sequences of NREM and REM sleep optimize both physical and mental recuperation as well as some aspects of memory consolidation that occurs during sleep, but this has not been confirmed.
Sleeping Positions
According to http://bettersleep.org/better-sleep/sleep-positions
There are three main sleeping positions with variables of each: side, back, and stomach. Sleep specialists recommend sleeping on your side in order to rest more comfortably and decrease the likelihood of interrupted sleep. While there are many variations of sleeping on your side, all of which are beneficial in helping to alleviate insomnia and chronic sleep deprivation, the most comfortable position involves bending the knees slightly upwards towards the chest area. For those with a bad back, consider placing a pillow between your legs to alleviate pressure on your hips and lower back. Sleeping on your side is actually encouraged for those suffering from back or hip pain or pregnant women since this position doesn’t increase pain in these areas.
If you prefer to sleep on your back, be careful as it may actually induce lower back pain and even episodes of apnea which interfere with normal sleep and restfulness. However, if you prefer to sleep on your back, there are a few minor alterations to this position that you can do to help sleep more soundly. Try placing a soft pillow or rolled up towel under your knees to facilitate the natural curve of the spine.
If you like sleeping on your stomach, you’re in for a bit of bad news…sleep professionals don’t recommend sleeping on your stomach as it causes strain on your lower back and possible neck pain. People who sleep on their stomach report increased restlessness caused by frequent tossing and turning in an effort to get comfortable. If you do sleep on your stomach use an extremely soft pillow or none at all so as not to put your neck at an awkward angle. For those with sleep problems, to begin with, it’s best not to sleep on your stomach.
 Fetus position – A whopping 41% of participants sleep in this curled-up manner. Women are twice as likely to rest like this and it is listed as the most common position. These sleepers are said to have a tough exterior but are still sensitive and may appear to be shy but warm up quickly.
Fetus position – A whopping 41% of participants sleep in this curled-up manner. Women are twice as likely to rest like this and it is listed as the most common position. These sleepers are said to have a tough exterior but are still sensitive and may appear to be shy but warm up quickly.
 Log position – If you sleep on your side with both arms down, you are a social, easy-going person who is trusting, sometimes to the point of being gullible. The study showed 15% of people sleep like a log.
Log position – If you sleep on your side with both arms down, you are a social, easy-going person who is trusting, sometimes to the point of being gullible. The study showed 15% of people sleep like a log.
 Yearner position – A close third is a side-lying position with both arms out in front of the body, with 13% of participants sleeping like this. Learners are noted to be open-minded and still cynical, suspicious, and stubborn about sticking to decisions once they are made.
Yearner position – A close third is a side-lying position with both arms out in front of the body, with 13% of participants sleeping like this. Learners are noted to be open-minded and still cynical, suspicious, and stubborn about sticking to decisions once they are made.
 Soldier position – These sleepers lie on their backs with arms down and kept close to the body. This 8% study is said to be reserved, quiet, without fuss, and hold themselves and others to a high standard. Soldier sleepers have a higher likelihood of snoring due to the flat-back position, which may not cause them to wake up often but may result in a less restful night’s sleep.
Soldier position – These sleepers lie on their backs with arms down and kept close to the body. This 8% study is said to be reserved, quiet, without fuss, and hold themselves and others to a high standard. Soldier sleepers have a higher likelihood of snoring due to the flat-back position, which may not cause them to wake up often but may result in a less restful night’s sleep.
 Freefall position – Those people who lie on their bellies with arms under or wrapped around a pillow with head turned to the side, makeup 7% of the population studied. Freefallers are brash, outgoing, and are very uncomfortable with criticism.
Freefall position – Those people who lie on their bellies with arms under or wrapped around a pillow with head turned to the side, makeup 7% of the population studied. Freefallers are brash, outgoing, and are very uncomfortable with criticism.
 Starfish position – Sleepers who lie on their backs with arms up near their head or the pillow account for 5% of participants. These people are good listeners, helpful, and are uncomfortable being the center of attention. People who sleep in starfish position are more likely to snore and to suffer from a poor night’s sleep more often.
Starfish position – Sleepers who lie on their backs with arms up near their head or the pillow account for 5% of participants. These people are good listeners, helpful, and are uncomfortable being the center of attention. People who sleep in starfish position are more likely to snore and to suffer from a poor night’s sleep more often.
The 3 Main Sleep Positions
Sleeping on Your Stomach
The Good
- Helps with digestion – I find this to be very true!
- Reduces symptoms of sleep apnea and prevents snoring
The Bad
- Causes neck pain when you turn your neck to the side
- Possibly suffocate and die if you don’t twist your neck – almost happened to me
- Wipes expensive moisturizer off your face and onto the pillow
- Pressure on your joints and muscles from a misaligned spine
- Potentially leads to pain, soreness, numbness, and tingling
I’m surprised this sleeping position isn’t more popular – only 7% of the population prefer to sleep like this – but I know I’m biased.
Sleeping belly down is good for cutting out the snoring but the negatives far outweigh any benefits it can bring. It’s arguably the worst position to sleep in for the many reasons listed above.
Even for massages, I’m wary of places that do not have elevated massage tables where there is a hole I can put my face when lying face down. Instead, they’d ask me to twist my neck to the side.
Good thing I don’t stumble on these places very often. When I do, I usually just walk right out. Usually, a proper massage table is an essential part of a Registered Massage Therapist’s toolbox.
Unfortunately, this IS my favorite position to sleep in and I do indulge from time to time, especially when my stomach isn’t feeling very well.
I don’t stay in it for too long – usually during the first 10-20 minutes of falling asleep. Then I turn over on my back to fall and stay asleep.